Rabies is expressed. Rabies in humans: signs and prevention of animal bites. How does rabies manifest in humans?
Rabies in foxes is extremely common. This is due to the peculiarities of their lifestyle. Quite often, these animals become the culprits of human infection. Even if people become infected with this deadly disease from a cat or dog, the primary source of infection is often a fox. After all, pets often get the virus when they encounter wild animals. Every person needs to know about the manifestations of this disease in foxes. This is especially necessary for those people who spend a lot of time in the forest, hunting or picking mushrooms. In addition, sick foxes often visit populated areas and can come close to humans.
What is rabies
Rabies is one of the most dangerous and deadly diseases that affects animals and people. The pathology is caused by a virus (Rabies virus), which affects the central nervous system. It causes irreversible changes in the brain, which are always fatal.
It is important to remember that the incubation period for this disease can be quite long. It ranges from 10 days to 3 months. Symptoms of the disease in humans can be divided into several stages:
- Often the disease begins with pain in the bite area, even if the wound has already healed. Then there is general malaise, a slight increase in temperature, anxiety, and insomnia.
- Heat stage. A person experiences strong light and sharp sounds. Convulsions appear, which are intensified by any irritants. Mental disorders are noted: delusions, hallucinations, and sometimes increased aggression. There is increased secretion of saliva.
- Period of paralysis. The patient's muscles paralyze the eyelids, cheekbones and legs. Taste distortions may occur when a person eats inedible objects. At this stage, the disease ends in death due to respiratory paralysis.
Modern medicine does not have drugs for rabies. Only a vaccination can save a person’s life, but it is effective only in the first 10 days after the bite. At the stage when the first signs of rabies appear, it is no longer possible to help the patient.
Why do foxes often get rabies?
Rabies in foxes is quite common. This is due to the way animals eat. Foxes eat small rodents, which are often carriers of the rabies virus. Infection occurs through the nutritional route, through the stomach. Humans are never infected this way. However, for animals this route of transmission of the virus is quite possible.

In addition, a small rodent can bite a fox in defense against it. In this case, the virus is transmitted in the most common way - through saliva. Sometimes foxes are attacked by larger predators and become infected when bitten. After all, it is very easy to detect a fox hole, and animals under the influence of the virus become aggressive.
Ways of transmission of the disease
From fox to man? Infection is possible only through contact of the saliva of a sick animal with blood. Most often this occurs with a bite. Infection is also possible when saliva gets on the skin with small wounds and when scratched. There are no other methods of infection.
Foxes can also be indirectly responsible for human rabies. Sick animals often attack stray dogs and cats, which subsequently infect people. A hunting dog can also be attacked by a rabid fox. In this case, the owner runs the risk of becoming infected from his pet. Therefore, it is very important to vaccinate dogs against this dangerous disease on time.
Seasonal periods of the disease
High incidence of rabies in foxes is observed during the following periods:
- From February to April. During this period there is always a large outbreak of the disease. This is due to the fact that in the spring the foxes go into rut. Fights often occur between males. Animals bite each other and transmit the virus.
- December. In winter, the fox population increases due to young individuals. This leads to a small outbreak of rabies.

After such periods, the incidence decreases somewhat, as many foxes die from rabies. But this does not exclude the possibility of infection. The danger of getting the virus from a fox exists in any season.
Appearance of a mad fox
How to determine rabies in a fox by appearance? This is quite difficult to do. The appearance of a sick animal may not have any obvious features, and at first glance it seems that the fox is healthy. However, you can notice some external signs of rabies in a fox:
- Profuse drooling with foaming and protruding tongue. These symptoms are observed at the height of the disease and are often accompanied by aggression of the animal.
- Unsteadiness of gait. Due to brain damage, the sick animal's coordination of movements is impaired.
- Squint, cloudy eyes, swollen muzzle. These signs are difficult to notice, since it is better not to approach a sick animal.
- Exhaustion. This sign is not specific for rabies. A fox can lose weight for other reasons.
Subsequently, due to developing paralysis, the animal’s limbs fail. However, in this state the animal can no longer lead an active lifestyle and attack a person. This is the final stage of rabies in foxes. A photo of the sick animal can be seen below.

Features of the behavior of a sick animal
It is much easier to determine the disease by the behavior of the fox. Pathology greatly affects the psyche and habits of the animal.
How does rabies manifest in a fox? First of all, the animal loses its instinct of self-preservation. It ceases to fear man. A healthy fox never approaches people or their homes. An animal with rabies freely approaches a person. Infected foxes often enter populated areas. This behavior is not typical for healthy animals.

With the violent form of rabies, the animal becomes aggressive. The fox barks in a hoarse voice. In this state, animals often attack people and animals.
However, it is no less dangerous when the disease occurs in a silent form. In this case, the animal looks calm and somewhat lethargic. It can approach a person without showing any signs of aggression and bite.
Unnatural affectionateness is one of the symptoms of rabies in foxes, which occurs in a quiet form. The animal approaches the person and begins to lick his hands. This may be followed by a sudden bite. It should be remembered that a fox is a wild animal, and affectionate behavior is uncharacteristic for such an animal.
Rabies in foxes is an insidious disease. After all, the animal becomes infectious during the incubation period, when no signs of pathology are observed. Therefore, in case of any fox bite, it is necessary to get a rabies vaccination as soon as possible.

How to behave when meeting a sick fox
What to do if you had to deal with a sick animal? It is necessary to behave extremely carefully so as not to provoke an attack and a fox bite:
- You need to stop immediately and not make sudden movements.
- You cannot turn your back on the animal and run away. Otherwise, the fox will give chase and attack from behind.
- You can't smile at the beast. When a person bares his teeth, animals take it for a grin.
- You should not show the animal that you are scared.
- You need to slowly move away from the fox with your back backwards.
- If the fox shows aggression and is about to attack, then you need to protect the throat area.
- If possible, you need to hide from the beast in some room or climb a tree.
- If the fox managed to knock you down, then you need to lie on your stomach and not move. It is necessary to cover your neck with your hands and your face with your elbows. Bites to these areas of the body are most dangerous.

What to do if you are bitten
If a fox bites, it is necessary to urgently treat the damaged area. The wound should be washed with soap and water or a hydrogen peroxide solution. Then you need to lubricate the bite site with iodine and bandage it. The same measures are necessary if there was no bite, but the animal’s saliva got on your skin.
Next, you need to immediately go to the nearest emergency room and undergo a rabies vaccination course. Doctors believe that it is best to start vaccinations in the first three days after the bite. The course of prophylaxis consists of six injections. Do not under any circumstances miss the next vaccine administration date and do not drink alcohol during vaccinations. This will help you save yourself from a deadly disease.
Article updated 09.27.2019
Over the past 3 years, 60 cases of human rabies infection have been recorded in Russia. The largest number of such cases are registered in the Central, Volga, North Caucasus and Southern federal districts, as well as in the Republic of Tatarstan and the Chelyabinsk region. In the Nizhny Novgorod region, quarantine has been declared today in 50 settlements. These municipal districts are recognized as unfavorable in terms of the spread of rabies, and among the sick there are both wild and domestic animals.
In September 2015, a quarantine was declared in 6 Moscow veterinary clinics due to the occurrence of rabies in domestic animals. If rabies was found in domestic animals, this is the most dangerous, since their contact with humans is likely.
Is rabies a fatal disease?
The rabies virus affects the central nervous system of animals and humans. Rising along the nerve pathways, it reaches the brain and causes inflammation (specific encephalitis). Until 2005, rabies was considered a fatal infection for humans. There are only a few known cases of people being cured of this terrible infectious disease. However, a timely vaccination or certain measures, which will be discussed later, can save the patient’s life.
The main carriers of the rabies virus are:
- Wild animals (wolves, foxes, wild cats, lynxes, bats, hedgehogs, rodents)
- Farm animals
- Pets
Statistics of rabies incidence in Russia by animal carrier species for 1997 - 2007
The diagrams show that the main sources of rabies are wild animals. Recently, due to the spread of rabies among wild animals, the virus penetrates simultaneously into several biological species. For example, it is transmitted from a wolf to a fox or marten. Therefore, you need to be especially careful and attentive in the forest. We previously wrote about.
Approximately half of all cases of rabies infection occur in domestic and farm animals that come into contact with wild animals. The most dangerous wild animals in terms of rabies infection are foxes (first diagram). Moreover, you can meet mad foxes both in the forest and in the city. When infected with rabies, foxes can manifest themselves in two ways. Some may behave aggressively and attack people. Others, on the contrary, are drawn to people and show affection, like domestic cats. This behavior is not typical for a healthy fox.
If you encounter such a fox, you must immediately leave the forest or area in which it is located. Under no circumstances should you pick them up.
How can a person become infected with rabies?
A person becomes infected with rabies when an animal attacks him and then bites him. When analyzing the bulletin on rabies, it was revealed that it is the street type of rabies that occurs on the territory of our country. 99% of people who died of rabies (WHO) were infected by street stray dogs. It is also possible to become infected with rabies when animal saliva comes into contact with damaged human skin.
The second source of human infection is forest foxes. If the saliva of an infected animal gets on forest edible grass (for example, sorrel, sorrel) or berries, then eating them unwashed can lead to infection. For prevention purposes, it is necessary to thoroughly wash any forest products.
You can become infected with rabies if a motorist hits an infected forest animal and touches dirty parts of the car or the animal itself with unprotected hands. Ideally, it is necessary to report the incident to specialists at animal disease control stations, who should treat the area with disinfectant solutions and impose quarantine. If the blood of, for example, a downed fox gets on a person’s skin, it is necessary to immediately go to the nearest emergency room.
In addition, humans can be infected by pets that have been bitten by rabid wild animals.
Symptoms of rabies in animals
Once a dog or cat is infected with rabies, it usually takes about 15 days before the animal begins to behave aggressively.
The most common symptoms in dogs are:
- Starts gnawing or licking the bite site.
- The dog's pupils dilate, and it begins to behave aggressively and even runs away from the house.
- While maintaining an appetite, the dog can swallow inedible things.
- The animal may have severe salivation with foam and vomiting (doctors consider this to be the main symptom of rabies).
- Hydrophobia (may not manifest itself).
After these signs appear, as a rule, on the third day, paralysis of all muscles and death of the animal occurs.
In cats The most common symptoms are salivation and intense agitation.
In cows limbs are paralyzed and death occurs.
Symptoms of rabies in humans
For rabies, the incubation period ranges from 8 days to 1 year. Most often, the disease does not manifest itself in any way for 40 days.
The duration of the incubation period and the course of the disease directly depend on the location of the bite on the body, the age of the victim, the depth of the wound and penetration of the virus, and the rapid use of the vaccine.
It is believed that the shortest incubation period for a person when bitten by a wolf. As for the location of the bite, the most dangerous are the injuries to the head, face and arms during an animal attack, since the rabies virus infects the nerve fibers and cells of a person, then moving along the spinal cord to the brain.
A person's death occurs due to suffocation and cardiac arrest.
Symptoms of rabies in humans:
- The primary symptoms of rabies include: low-grade body temperature (above 37, but below 38 degrees), malaise, convulsions during breathing and the desire to swallow food, headache, nausea, lack of air. The bite site turns red, and increased salivation is observed.
- Nervous excitement, irritability, anxiety, headache, insomnia, depression, and poor appetite appear. All this lasts approximately 1-3 days.
- Then a characteristic symptom of rabies appears - “foaming at the mouth”; excitement is accompanied by muscle cramps, which can occur even from bright light. Patients may become aggressive, scream, tear their clothes, use force, and break furniture. Body temperature rises to 39-41 degrees, tachycardia, increased lacrimation, salivation, and sweating are observed.
- Subsequently, hydrophobia and severe breathing spasms appear. Most often at this moment the pupils dilate, and convulsions can distort the face.
- Then the face turns blue. At the last stage of the disease, hallucinations with changes in mood and attacks of anger, which are very dangerous, are possible. During a rage, a sick person may even bite others.
It's worth knowing that there is " quiet fury" When a person’s illness can be practically asymptomatic, he does not show agitation. It is most often transmitted by the bite of humans by bats found in South America.
What to do if you are bitten by a rabid animal or a stray dog?
- At the first symptoms of rabies, it is almost impossible to save a person. Therefore, if you are bitten by a forest or stray animal, or by an unvaccinated pet, you should immediately seek medical help.
- If the rabid animal is domestic, then it must be tied up and isolated.
- Before the ambulance arrives, wash the wound with water and laundry soap and cause profuse bleeding from the wound, as there is a possibility that the virus will come out of it in the blood (virus penetration is 3 mm per hour)
- You cannot stitch the wound, treat it with alcohol, iodine, or any other antiseptic.
- You should not drink alcohol after a bite.
- Animals that have bitten people should be examined by a veterinarian.
- If the animal is aggressive and there is no way to tie it up, then it is necessary, without touching it, to call the sanitary service through the rescue telephone number 112.
Prevention of rabies
In the prevention of rabies, a very important role is played by the owner's compliance with the rules for keeping pets. The very first thing you need to do when you decide to take an animal into your home is to find out if it is vaccinated against rabies. Preventive vaccination using rabies vaccines for pets is mandatory in our country, and in any city or town, even a small one, they are required to do it free of charge in state veterinary clinics. The rabies vaccine is given at an early age. Repeated vaccinations must be carried out every year.
If you suspect your pet has rabies, you should immediately take it to a veterinarian for examination and testing. If an animal is not vaccinated, then it should not be allowed to participate in exhibitions and livestock farms, or go hunting with it in the forest.
If you want to sell, buy or transport dogs, you must obtain a veterinary certificate indicating that the animal was vaccinated against rabies no more than 11 months and no less than 30 days before the trip.
If your pet has been bitten by wild animals or stray dogs, you must immediately report this to the veterinary services so that it can be examined by a doctor.
The material was prepared with the participation of a veterinary paramedic
Rabies is an acute infectious disease of humans and animals that affects the central nervous system. Its cause is viruses that have a tropism for the tissues of the nervous system, where, after biting a sick animal, they move at a speed of 3 mm per hour. After replication and accumulation in the tissues of the central nervous system, viruses spread through neurogenic pathways to other organs, most often to the salivary glands.
The incidence of the disease depends on the location and severity of the bite. In 90% of cases, the disease develops with bites on the neck and face, in 63% - in the hands, in 23% - in the shoulder. The signs and symptoms of rabies at all stages of the disease are highly specific. There are no effective treatments for the disease. The disease is usually fatal. Timely vaccination against rabies is the most effective prevention of the disease. The rabies vaccine was first obtained in 1885 by the French microbiologist Louis Pasteur. And in 1892, Victor Babes and in 1903 A. Negri described specific inclusions in the neurons of the brain of animals that died from rabies (Babes-Negri bodies).
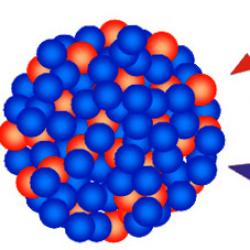
Rice. 1. The photo shows rabies viruses.
Rabies virus
The filterable rabies virus is a member of the genus Lyssavirus(from the Greek lyssa, which means rabies, demon) family Rhabdoviridae.
The rabies virus has a tropism for nervous tissue.
- Rabies viruses are heat sensitive. They are quickly inactivated when exposed to solutions of alkalis, iodine, detergents (surfactant synthetic substances), and disinfectants (Lysol, chloramine, carbolic and hydrochloric acids).
- Viruses are sensitive to ultraviolet irradiation, die quickly when dried, and die within 2 minutes when boiled.
- At low temperatures and freezing, rabies viruses persist for a long time. They can be stored in animal corpses for up to 4 months.
Viruses are transmitted to humans through bites with saliva or through damaged skin that contains saliva from a sick animal. Damage to the central nervous system inevitably leads to the death of the patient. The presence of viruses in the central nervous system is indicated by the detection of “Babes-Negri bodies” in ganglion cells.

Rice. 2. The photo shows rabies viruses that resemble a bullet in appearance. One end is rounded, the other is flat. The synthesis of viral particles occurs in the cytoplasm of neurons.

Rice. 3. The photo shows the rabies virus. The virion is surrounded by a double shell. On the outer shell of viral particles there are spikes (protrusions) with knobby swellings at the ends. Inside the virions there is an internal component, which is a thread-like formation. The photo clearly shows transverse stripes representing a nucleoprotein.
Taurus Babesha-Negri
In 1892, V. Babes and in 1903, A. Negri, described specific inclusions in the cytoplasm of neurons in the brains of animals that died from rabies. They are called Babesh-Negri bodies. Large neurons of the ammon's horn, pyramidal cells of the cerebral hemispheres, Purkinje cells of the cerebellum, neurons of the thalamus optic, cells of the medulla oblongata and ganglia of the spinal cord are areas of the nervous system where Babes-Negri bodies are most often found.
Cytoplasmic inclusions are strictly specific for rabies disease
Babes Negri bodies are detected in the neurons of the brain of dogs that died from rabies in 90 - 95% of cases, in humans - in 70% of cases.
According to a number of researchers, Babes Negri bodies are:
- places where virions replicate
- places where the production and accumulation of the specific antigen of the rabies pathogen occurs,
- The internal granularity of Babes-Negri bodies represents viral particles associated with cellular elements.

Rice. 4. The photo shows nerve cells with cytoplasmic inclusions. Babes Negri bodies have different shapes - round, oval, spherical, amoeboid and fusiform.

Rice. 5. The photo shows the Babesh-Negri body. The internal granularity of the inclusions represents viral particles associated with cellular elements.

Rice. 6. The photo shows the Babes-Negri body in the light of a conventional microscope. They are surrounded by a light rim.
Replication of viral particles in rabies is always accompanied by the formation of specific inclusions - Babes-Negri bodies.
Epidemiology
Articles in the "Rabies" sectionMost popularRabies (from Latin rabies; obsolete hydrophobia or hydrophobia) is the name of a deadly infectious disease caused by the rabies virus entering the human body.
Its carriers are animal carriers, which infect a person by biting, scratching or salivation (the infection is contained in saliva). In the old days, it was believed that a sick person was possessed by evil spirits, demons. This is where the name “rabies” comes from.
Every year around the world, about 50 000 Human.
Wild animals that can become carriers of rabies:
- foxes;
- martens;
- raccoons;
- the bats;
- jackals.
Pets can also become carriers of the virus:
- dogs;
- cats;
- agricultural animals.
There is a theoretical possibility of transmission of the virus from person to person through a bite (not confirmed).
Rabies in humans after being bitten
The virus enters the body when it enters saliva animal into a wound or any other scratch on the skin (less often on the mucous membrane of the eyes or mouth) and through nearby muscle fibers it is introduced into the nervous tissue.
It reaches the following parts of the human body, disrupting their functioning:
- salivary glands;
- nerve cells;
- cortex;
- hippocampus;
- bulbar centers;
- spinal cord.
The body of the virus is unstable to high temperatures (above 56 ° C) and does not tolerate ultraviolet rays, but ignores the effects of antibiotics. However human organism- an ideal environment for its reproduction.
If after a bite the wound is not treated properly, the infection can spread throughout the body.
Nerve fibers act as a platform for further division of the virus and its advancement (passes through axons, forming Babes-Negri bodies). It ends its path in the cerebral cortex and spinal cord centers, leading to meningoencephalitis. The causative agent of the disease, moving along nerve fibers, also provokes the development encephalitis(inflammation of the central nervous system).
During its movement through the body, the virus provokes the following pathological changes in nervous tissue:
- dystrophy;
- necrosis;
- inflammation.
If prompt measures are not taken, these violations will lead to of death sick. Death occurs due to suffocation or cardiac arrest.
First signs
Recognizing the first signs of infection is an important task for further treatment. If you detect the disease in its initial stages and consult a doctor, the chances of recovery increase significantly.
A person infected with rabies may experience cold-like symptoms in the early stages:
- the appearance of fever;
- headache;
- muscle pain;
- loss of appetite;
- nausea;
- prostration.
In the future, the symptoms will progress and you need to focus on the following signs:
- increased temperature after a bite (up to 40.5° C);
- delusional states;
- hallucinations;
- anxiety and agitation;
- cramps and tingling in the bite area.
If no changes are observed after the bite, in any case you should contact to the doctor: The animal could be a carrier of other infections and diseases.
How long does it take for them to appear?
Rabies has its own incubation period. It often takes time for the first signs of a disease to appear - from 1 to 4 months. Sometimes it is enough for the development of pathology 10 days, and sometimes it takes a year to pass.
There is a known case when the period from the virus entering the body to the development of symptoms was 6 years. Such a long incubation period is explained by the fact that the virus moves through the body along nerve fibers and not through blood vessels, which significantly delays the manifestation of the clinical picture.
The timing of rabies manifestation also depends on the following factors: 
- type of animal infected;
- amount of virus;
- immunity strength;
- localization of the bite (the most dangerous places are those with a wide network of nerve endings - hands, genitals, head).
Phases
Observations of the disease allowed us to identify 3 main phases of its course:
- Premonitory.
- The height of
- Stage of paralysis.
The development of the disease is not always unambiguous and does not always maintain exactly this sequence. There are cases when rabies debuted immediately with third stage(paralytic rabies) or was limited to symptoms only second stage(violent rage).
The total duration of the disease is 8-12 days.
Prodromal stage (3 days) characterized by a slight increase in body temperature (up to 37.3° C). The patient experiences inexplicable anxiety and sleep disturbances. The healed wound left by the bite begins to hurt.
In full swing (4 days) There is an increase in sensitivity, the muscles cramp. Hydrophobia and aerophobia arise. Patients are visited by a feeling of fear, they become irritable and aggressive.
At the final stage paralysis (last days) the person is completely immobilized, asphyxia occurs.
Symptoms of rabies in humans
Symptoms develops only after the virus has spread throughout the body.
The classic manifestations that accompany the disease are as follows:
- Change in behavior:
- irritability;
- aggressiveness.

- excessive excitement;
- muscle spasms;
- uncontrolled movements of the diaphragm and respiratory muscles;
- unnatural poses;
- convulsions;
- weakness;
- paralysis.
- Cognitive impairment:
- confusion in thoughts;
- hallucinations;
- rave.
- Problems with perception:
- photosensitivity;
- hypersensitivity to touch and sound;
- visual impairment;
- aerophobia;
- rabies.
- Disorders of the salivary and lacrimal glands:
- increased salivation;
- lacrimation;
- difficulty swallowing;
- foaming at the mouth.
Symptoms may not don't make yourself known in the case of a small amount of virus entering the body.
Treatment of rabies in humans
Call a doctor immediately after contact with a possible carrier rabies– the main rule with which successful treatment of the disease begins.
While waiting for a specialist, it is necessary to take a number of preparatory actions:
- Within 10 minutes wash the bite site with soap.
- Treat the wound alcohol or iodine.
- Tie on the damaged one area of bandage or clean gauze.
- Notify the veterinary clinic that a potentially dangerous animal is walking around in the vicinity (its capture is necessary to establish the status of the carrier of the infection).
- If you know its owner, provide his contact information to the veterinarian (this will make it easier to capture the pet and then place it in quarantine).
A diagnostic procedure is usually not required to confirm rabies. It is sufficient for a specialist to examine the infected person and textbook symptoms(hydrophobia, aerophobia) get an idea of the picture of the disease. Recent advances in diagnostics make it possible to detect rabies antigen on the upper layers of the eyeball.
There is a cure for rabies - a vaccine developed in 1885 by Louis Pasteur. However, the likelihood of recovery decreases with every second of delay. The vaccine should be administered before symptoms appear (it is best to be vaccinated in advance for prevention purposes). The injection is made into the soft tissue in the bite area.
The promptness of medical intervention determines the outcome of the disease. In combination with the vaccine, experts use additional medications.
So, modern medicine has the following tools to rid a patient of the virus:
- Louis Pasteur vaccine;
- anti-rabies serum;
- anti-rabies immunoglobulin.
Vaccination is carried out in several stages: 
- on the day of application;
- on day 3;
- on day 7;
- on day 14;
- on day 30;
- on day 90.
Until 2005, treatment of the disease was considered impossible at the stage of signs of rabies appearing. After the clinical picture manifested itself in the patient, doctors were limited to symptomatic treatment (use of sedatives, curare-like drugs, artificial respiration). However, modern research has made it possible advance in the study of the disease.
Variable success in treatment at the stage of symptom development (5 cases of recovery in 37 infected in 2012) was demonstrated by scientists from the USA, using the so-called. Milwaukee protocol - placing the patient in a coma and administering a combination of pharmacological agents:
- antiviral drugs;
- sedatives;
- anesthetics;
- immunostimulating drugs.
In world practice, only 8 cases favorable outcome after a long stay of the virus in the human body. One of them is the recovery of Gina Gies, who was artificially put into a coma by American specialists.
This is the essence of the method "Milwaukee Protocol"- using a coma to reduce the activity of the nervous system, in the hope that in this state the body will independently begin to produce antibodies. This treatment method still remains experimental.
Prevention of rabies
Preventive measures:
- Vaccination animals.
- Walkthrough course of preventive vaccinations for humans (immunization).
- Limitation in the consumption of alcohol and individually intolerant foods during the period of human vaccination.
- Limitation physical activity during the course of treatment.
- Finding in hospital in case of serious condition or pregnancy.